The Invisible Wound -The Silent Struggle
Understanding Head Injuries Among First Responders
Don’t be afraid, for I am with you. Don’t be discouraged, for I am your God. I will strengthen you and help you. I will hold you up with my victorious right hand.
Isaiah 41:10
Have you ever had your “bell rung”? Have you ever been hit in the head and felt dazed and confused afterward? Head Injuries have been increasing and gaining much attention, especially in amateur and professional sports. But what about our first responders? They, too, are not immune to the risks of head injuries. Firefighters, law enforcement officers, and emergency medical service personnel face these daily dangers. Only about ten years ago did the Department of Defense (DoD) start to recognize the importance of treating head injuries. A 2023 DoD report states that from 2000 to 2022, roughly 458,894 Service members were diagnosed with a Traumatic Brain Injury (TBI) during training or in combat.
What is TBI, and how does it affect First Responders? TBI has three classifications depending on the severity of the head injury: concussions or mild TBI (mTBI), moderate TBI, and severe TBI.
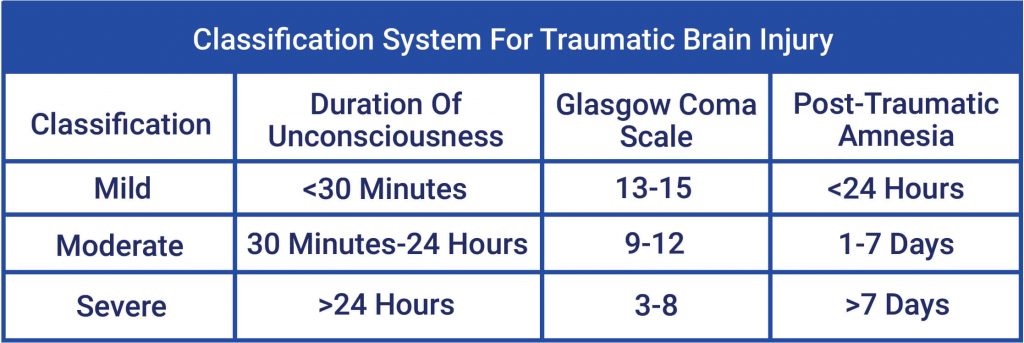
Figure 1 Courtesy of Verdugo Psychological Services
The American Association of Neurological Surgeons defines a concussion as:
“an injury to the brain that results in temporary loss of normal brain function. Medically, it is defined as a clinical syndrome characterized by immediate and transient alteration in brain function, including alteration of mental status or level of consciousness, that results from mechanical force or trauma.”
Memory, judgment, reflexes, speech, balance, and muscle coordination can all be impacted by a concussion. People who have suffered concussions often experience a brief period of amnesia or forgetting, during which they are unable to recall events that occurred just before or after the injury. Other symptoms of TBI can include headaches, dizziness, nausea, and sensitivity to light and sound.
According to the Centers for Disease Control, in 2020, there were an estimated 214,110 TBI-related hospitalizations. In 2021, there were 69,473 TBI-related deaths, representing 190 TBI-related deaths per day. Those numbers do not include those treated in emergency rooms, primary care, and urgent care facilities, or the untreated.
Even though concussions are common in the general population, First Responders seem to have been passed over when it comes to TBI education and treatment. Among First Responders, head injuries are common. Firefighters are exposed to ceiling, roof, and building collapses. They also experience slips, trips, and falls, risking head injuries. Law Enforcement Officers have a high risk of injury through assaults, traffic accidents, and a variety of other job-related activities.
In the National Library of Medicine publication “Psychological Distress and Line-of-duty Head Injuries in Firefighters,” researchers discovered that head injuries are common among firefighters; however, very little data is available on the relationship between mTBI and Post Traumatic Stress injury (PTSi). Researchers found that 76% of firefighters in the study reported at least one head injury in their lifetime. Firefighters who sustained a head injury while on duty showed notably worse symptoms of PTSi than both firefighters without a head injury and firefighters whose head injury did not occur while performing their duties.
Among Law Enforcement, the numbers are similar. A recent study conducted by The Ohio State University and published in the Journal of Head Trauma Rehabilitation showed that seventy-four percent of those in the study had suffered from a head injury during their lifetime. Over half of those surveyed sustained a head injury leading to a loss of consciousness, confusion, or memory gaps. Fifty-seven percent of the officers reported that their work-related head injury hindered their ability to perform their jobs. Sadly, 24% said they received no treatment or support from their organization after the injury.
The study concluded that head injuries resulted in higher long-term symptoms of depression and PTSi. And that many head injuries are undiagnosed and untreated. The study suggested that Law Enforcement Officers do not receive the organizational backing they require to heal from workplace injuries, which affects their ability to perform their duties.
It has been well-documented that many cops and firefighters suffer from PTSi, and some may self-medicate with alcohol or drugs. There is a complex and significant relationship between substance abuse and TBI. TBIs have been linked to an increased risk of drug and alcohol abuse. Head injuries often change the chemical balance and functions in the brain. Traumatic Brain Injury survivors are more susceptible to developing alcohol use disorders. This is partly due to alcohol abuse as a means of dealing with psychological trauma. The abuse of alcohol and other drugs will interfere with the healing process and, in many cases, worsen TBI symptoms.
While the surveys done on our firefighters and cops may be small, there has been substantial research involving our active-duty military and Veteran communities. A July 2023 article in the JAMA Network, Associations of Military-Related Traumatic Brain Injury With New-Onset Mental Health Conditions and Suicide Risk, showed that “soldiers with a history of TBI had a 31.9% increase in alcohol use disorders” and a 100% increase in substance use disorders.
The study also indicated that of the 108,785 soldiers diagnosed with TBI, 458 (0.4%) died by suicide.
Suicide is a significant public health concern; according to a study published by the National Library of Medicine, those with a history of TBI have a 1.55 to 4.05 times higher suicide rate compared to the general population. In an August 2023 publication by the Defense Suicide Prevention Office, researchers found that “Patients who have experienced a mild TBI have a twice as high risk of suicide than individuals without mild TBI. Patients with mild TBI also appear to have a higher risk of suicide attempt and suicidal ideation.”
Researchers created timelines for those Veterans who died by suicide and learned that those who suffered from TBI died by suicide 21% sooner than those without TBI after returning from deployment. Soldiers with TBI and diagnosed with a substance use disorder died by suicide 63% sooner than those without.
TBI and Dementia
Research has shown that early or midlife traumatic brain injury is associated with an increased risk of dementia in later life. According to the National Library of Medicine, about 2% of the U.S. population suffers from long-term disabilities due to a prior TBI injury. In a study by the Institute of Medicine, researchers found that there is enough data to conclude that dementia and moderate-to-severe traumatic brain injury are related.
Researchers from the Perelman School of Medicine at the University of Pennsylvania found that head injuries are long-lasting and that dementia could develop later in life after a single head injury.
Chronic Traumatic Encephalopathy
Caused by repeated head injuries, Chronic Traumatic Encephalopathy (CTE) is a neurodegenerative disorder. Currently, the only way to diagnose CTE is after the person has died and an examination of the brain is conducted. CTE has been found in athletes participating in combat sports such as boxing, mixed martial arts, and kickboxing. Contact sports such as American football, rugby, professional wrestling, ice hockey, and soccer (heading the ball) have also been linked to CTE.
After a Boston University CTE Center study, The National Football League (NFL) acknowledged that CTE is an issue in the NFL. The study found that 345 of the 376 players studied were diagnosed with CTE.
Junior Seau, Aaron Hernandez, Phillip Adams, and Jovan Belcher are just some of the NFL players who died by suicide and were diagnosed with CTE postmortem.
Amyotrophic Lateral Sclerosis (ALS, or Lou Gehrig’s disease) and CTE may have a possible connection. According to the ALS Association, military veterans diagnosed with CTE are twice as likely to have ALS. Though 4–6% of CTE cases go on to show clinical or pathological ALS features, a condition known as CTE-ALS, the connection between CTE and ALS remains unclear.
CLF HelpLine for Law Enforcement & First Responders
Created by the Concussion Legacy Foundation and CopLine, The CLF HelpLine provides individualized support to families and individuals dealing with the aftermath of brain injury.
If you or a loved one recently had a concussion, are experiencing persistent symptoms, or are concerned about chronic brain injury, please get in touch with the CLF HelpLine.
As First Responders, we swore to protect good and fight evil. Many have lost track of their priorities and have put the job first in their lives. If you are experiencing lower than usual sense of self-worth, depression or misplaced guilt, inability to specifically remember or talk about the trauma, feeling numb emotionally, dissociation (not aware of the present moment), a feeling of disconnection from your everyday lives, feeling hyper-aroused and vigilant for danger all the time, lashing out in irritability or unexplained anger, feeling jittery, or unable to concentrate on tasks at hand or other anxiety disorders, such as panic or intense distress, talk to someone and get help. Return to the basics: Put God First, Family Second, and the job further down in the order.
IF YOU HAVE THOUGHTS OF SUICIDE, GET HELP NOW
Law Enforcement Copline (800) 267-5463
Firefighters / Medics Fire/EMS HELPLINE (800) 731-FIRE (3473)