Cardiovascular Disease
Beloved, I pray that all may go well with you and that you may be in good health, as it goes well with your soul. 3 John 1:2
As first responders, we address medical emergencies, fight fires, and protect the public, spending days and nights watching out for everyone. But for many of us, we do not look out for ourselves. Cardiac arrest, heart attack, stroke, and heart failure are all part of cardiovascular disease. Heart-related disease is the leading cause of death in the United States; according to the Centers for Disease Control, one person dies every 33 seconds, accounting for one in every five deaths[1] and costing 239.9 Billion dollars per year.[2] According to the American Heart Association, in the United States, someone suffers from a heart attack every 40 seconds.[3]
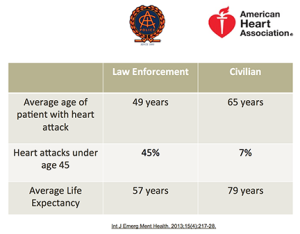
Dr. Jonathan Sheinberg is a Board-Certified Cardiologist, an expert in cardiovascular disease, and a Lieutenant on the Cedar Park (TX) Police Department. He is also the founder of the Public Safety Cardiac Foundation. His research has shown that “the life expectancy of a public safety officer is almost 20 years less than that of a civilian counterpart. The average life span of a civilian is 79 years old. For a police officer, it is 57, and it gets worse. The average age for a cardiac event in the civilian population is 65. For a cop, it is 45. The risk of sudden cardiac death increases by 18 times when first responders reach the age of 45. That risk is even higher with hypertension and smoking.”[4] In an article by Scott Eskwitt from Cordico, Eskwitt explains that 55% of firefighter line-of-duty deaths are due to stress, overexertion, heart attacks, and strokes.
The sad fact is, on average, a police officer lives 15 years less than the average American. Nearly 50% of police officers will die from heart disease within five years of retirement, and statistically, cops are 25 times more likely to suffer a heart-related injury or death than from a suspect’s aggressive actions.
According to the National Fire Protection Administration, “A total of 36 firefighters died as a result of sudden cardiac deaths in 2022. Of this total, 20 deaths occurred while firefighters were on duty (the traditional count), and 16 deaths occurred within 24 hours of duty. Career firefighters accounted for 14 of the sudden cardiac deaths and volunteer firefighters for 22 of the deaths.” Since 1977, the majority of firefighter deaths have been attributed to sudden cardiac death. About 88% of paramedics reported at least one significant cardiovascular risk factor
WHY DO FIRST RESPONDERS HAVE AN INCREASED RISK OF HEART DISEASE?
Overactive nervous and endocrine systems
 While an average person may only experience less than a dozen traumatic incidents in their lifetime, first responders may experience that in one shift. Over a 30-year career, first responders will encounter thousands of stressful incidents. These incidents stay in our minds, not letting us forget what our bodies feel or what our eyes have seen. This all leads to depression, Post-Traumatic Stress, and suicidal ideation. After all, how will the body react if the mind cannot correctly handle the traumas that occur every day?
While an average person may only experience less than a dozen traumatic incidents in their lifetime, first responders may experience that in one shift. Over a 30-year career, first responders will encounter thousands of stressful incidents. These incidents stay in our minds, not letting us forget what our bodies feel or what our eyes have seen. This all leads to depression, Post-Traumatic Stress, and suicidal ideation. After all, how will the body react if the mind cannot correctly handle the traumas that occur every day?
The body’s nervous and endocrine systems release hormones that regulate mood, metabolism, growth, development, reproduction, and organ function. When you experience a traumatic event, your body’s physiological response kicks into action. You go into the fight-flight-freeze response. This response is your body’s way of helping you cope with danger. This response starts in the brain’s hypothalamus, setting off changes in your nervous and endocrine systems.
As hormones are released into your body, your heart rate speeds up, your blood pressure rises, and your pupils dilate. Your muscles tense up as more blood is diverted to them, and your lungs absorb more oxygen. You focus on the threat, diminishing your attention to less important tasks. Your body releases high levels of adrenaline, cortisol, and dopamine during every high-stress situation. During a regular shift, first responders experience these responses several times. Your glands, which create these stress hormones, are constantly exhausted and burned out without enough sleep, relaxation, exercise, or a balanced diet to recover.
Sleep deprivation
It has been well-documented that first responders are sleep-deprived. Sleep is one of God’s greatest gifts, a time when our bodies can rejuvenate. While mainly affecting those who work rotating shifts, it is a problem with the 2 million first responders in the United States.
Created by a consistent lack of sleep or reduced quality of sleep, sleep deprivation puts a drain on your mental and physical abilities. Sleep deprivation leads to loss of productivity, poor decision-making, psychological & physical health problems, anxiety, depression, paranoia, and a higher risk of death. A lack of sleep negatively affects your body weight and can lead to a higher risk of type 2 diabetes. Not sleeping enough keeps your blood vessels from healing, changing your blood pressure, and increasing your risk for cardiovascular disease. Sleep loss decreases male hormone production, including growth hormones and testosterone.
Sleep expert and West Point Psychologist Lt. Col. Dave Grossman stated: “Sleep deprivation is the Number 1 reason officers commit suicide, make ethical mistakes, and use excessive force.”[5]
Caffeine addiction
Because first responders are sleep-deprived, many compensate by using caffeine. Caffeine is the most commonly used drug in America. It is a central nervous system (CNS) stimulant that alters mood and behavior and accelerates the flow of information between the brain and the body. Coffee temporarily inhibits the hormones in your body that encourage sleep, giving you more energy and alertness. Along with increasing your heart rate and metabolism, caffeine may increase your urine and stomach acid production.
Caffeine overuse, especially in energy drinks, can cause “atrial fibrillation,” a kind of arrhythmia or irregular heartbeat. If left untreated, severe cases of atrial fibrillation can lead to palpitations, clots, heart failure, and stroke.
Energy drinks contain large amounts of caffeine; many have ingredients like guarana that enhance the effects of caffeine or other stimulants. Energy drinks are loaded with sugars and legal stimulants such as taurine and L-carnitine.
Lack of fitness, poor nutrition, and obesity
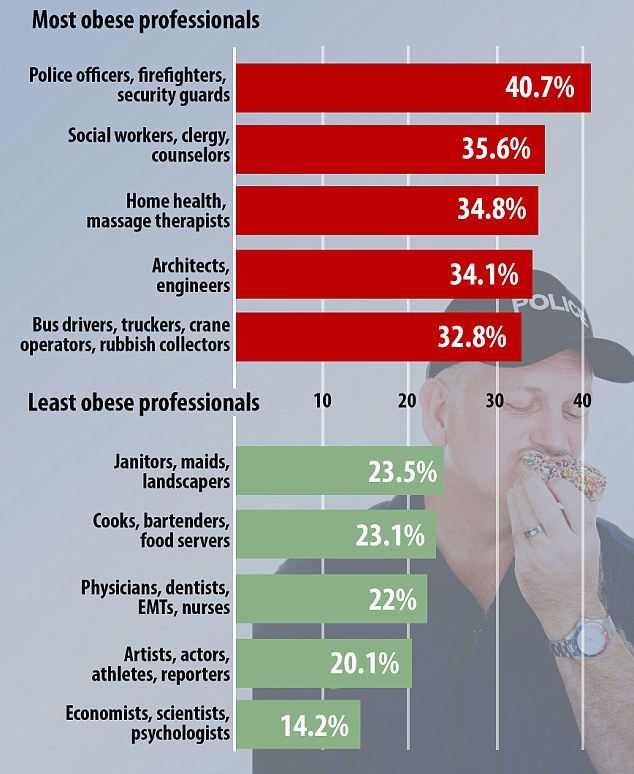
photo courtesy DailMail.com
Being a first responder requires a higher level of physical fitness than other occupations. Within law enforcement, it is estimated that 80% of our officers are overweight, and about 40% are obese. Several studies found that the prevalence of overweight and obesity combined is very high in the career fire service, ranging from 73% to 88%. Similar prevalence estimates (76% to 87%) have been documented for volunteer firefighters.[6]
Numerous related conditions, such as higher rates of diabetes and hypertension as well as a higher chance of musculoskeletal injuries, are often brought on by obesity. Police officers who are overweight may encounter increased hostility and even physical assault, potentially decreasing their ability to perform in the field. Among firefighters, only about 30% of those who were obese sought medical assistance in weight loss.
Numerous diseases, including depression, osteoarthritis, Type 2 diabetes, obstructive sleep apnea, cardiovascular disorders, and certain types of cancer, are made more likely by obesity.
Shift work, poor and unhealthy eating habits, job stress, sleep disorders, and the lack of fitness standards are all factors that may cause weight gain. The majority of police officers in this country eat as poorly as most others. Due to tight schedules, cops often grab something on the go and hit the streets. Many officers rarely have time for a proper and healthy meal, even in their personal lives.
The Solution
Cardiovascular disease is a major problem in the first responder community, and it is generally preventable. Diet and exercise are two of the most fundamental activities for maintaining a healthy lifestyle. Getting “checked” by seeing your primary care physician is something we must do to detect and prevent heart disease. Dr. Jon Sheinberg has identified three procedures for first responder early screening:
- Imaging Modality
- Coronary artery calcium scoring: This is a low-dose CT scan that identifies plaque build-up through measuring calcium levels in the heart.
- Carotid ultrasound: This test is a very simple, non-invasive early screening that allows doctors insight into early plaque build-up and inflammation in arteries of the neck.
- Coronary Inflammatory Markers: These markers do not indicate all-body inflammation but are specific to the cardiovascular system.
- Lp-Pla2 markers
- Oxidized LDL
- Standard or Advanced Lipid Panel: Everybody needs to have their cholesterol checked. However, typical cholesterol testing using the range for the general population do not always reveal the risk first responders have for cardiac issues, underscoring the need that cholesterol testing should be paired with other screening modalities.[7]
It is imperative that agencies safeguard their people from heart disease. The Commission on Accreditation for Law Enforcement Agencies (CALEA) estimates that an in-service heart attack costs between $450,000 and $750,000 per event. In contrast, it is estimated that department-mandated screening for heart disease could save the agency about $5,000 per year.
It is recommended that agencies offer cardiac screenings to their employees once every one to two years. This will ensure that employees maintain good health and any potential cardiac issues are detected early on. In addition to saving lives, this would stop costly worker’s compensation claims. Mobile heart screening programs provide the latest in screening technology and are cost-effective.
Agencies should also promote a healthy culture. Employees should be allowed and encouraged to work out on duty. Most police stations and firehouses have workout equipment or gyms. In order to motivate people, it’s important to offer incentives. While some may not prioritize their well-being, everyone likes a pay incentive. Leaders who prioritize their health show care for themselves and their employees.
We need to take care of ourselves. We need to be proactive. Get yearly bloodwork, get your heart screened, and get those yearly physicals. Do some type of aerobic activity; one of the most significant benefits of exercising thirty minutes a day is reduced risk of diseases. Exercising strengthens your heart and improves blood circulation. The enhanced circulation or increased blood flow raises oxygen levels in the blood. This helps lower your risk of heart disease and associated risk factors. These are high cholesterol, high blood pressure, stroke, heart attack, high triglyceride levels, and coronary heart diseases.[8]
As First Responders, we took an oath to protect good and fight evil. Many have lost track of their priorities and have put the job first in their lives. If you are experiencing lower than usual sense of self-worth, depression or misplaced guilt, inability to specifically remember or talk about the trauma, feeling numb emotionally, dissociation (not aware of the present moment), a feeling of disconnection from your everyday lives, feeling hyper-aroused and vigilant for danger all the time, lashing out in irritability or unexplained anger, feeling jittery, or unable to concentrate on tasks at hand or other anxiety disorders, such as panic or intense distress, talk to someone and get help. Get back to the basics Put God First, Family Second, and the job further down in the order.
You made all the delicate, inner parts of my body and knit me together in my mother’s womb. Thank you for making me so wonderfully complex! Your workmanship is marvelous-how well I know it. Psalm 139:13-14
-
National Center for Health Statistics. Multiple Cause of Death 2018–2021 on CDC WONDER Database. Accessed November 6, 2023. ↑
-
National Center for Health Statistics. Percentage of coronary heart disease for adults aged 18 and over, United States, 2019—2021. National Health Interview Survey. Accessed November 6, 2023. ↑
-
Tsao CW, Aday AW, Almarzooq ZI, Beaton AZ, Bittencourt MS, Boehme AK, et al. Heart Disease and Stroke Statistics—2023 Update: A Report From the American Heart Association. Circulation. 2023;147:e93–e621. ↑
-
Cordico. Understanding Cardiovascular Risks to First Responders – Cordico, Accessed November 6, 2023. ↑
-
McCrabb, Rick, “Expert: There is no room for “tired cops,’ Dayton Daily News, published September 1m 2017, https://www.daytondailynews.com/news/expert-there-room-for-tired-cops/VkZY4nHJLZRiXUQvSZGawO/ ↑
-
Poston, Walker S.C. Ph.D., The Prevalence of Overweight, Obesity, and Substandard Fitness in a Population-Based Firefighter Cohort, accessed November 14, 2023, https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=21386691 ↑
-
Cordico. Understanding Cardiovascular Risks to First Responders – Cordico, Accessed November 6, 2023. ↑
-
R. Mogeni, “30 Mins of Cardio A Day; The Good, The Bad, And the Myth,” accessed November 20, 2023, https://betterme.world/articles/30-mins-of-cardio-a-day/ ↑